- 4.0 - 8.0 CE Credit Hours
- For Pediatric Responders
- Includes Videos, Megacode Scenarios, Practice Tests & More
The neurological examination assesses the nervous system, coordination, balance, sensory perception, motor dysfunction, and more. The providers implement targeted interventions such as conducting CT (Computed Tomography) scans, administration of fibrinolytic agents, assessment of ABCs, and readiness for transition to care for invasive interventions, if needed. The algorithm framework also contains a visual flowchart that shows an organized path to help healthcare professionals manage stroke cases successfully. Following in a flowchart of ACLS Suspected Stroke Algorithm.

Online PALS certification and recertification
- Compliant with ECC and OSHA guidelines
- Nationally accepted course
- Available anytime, anywhere
- Earn CE credit hours
$119.00
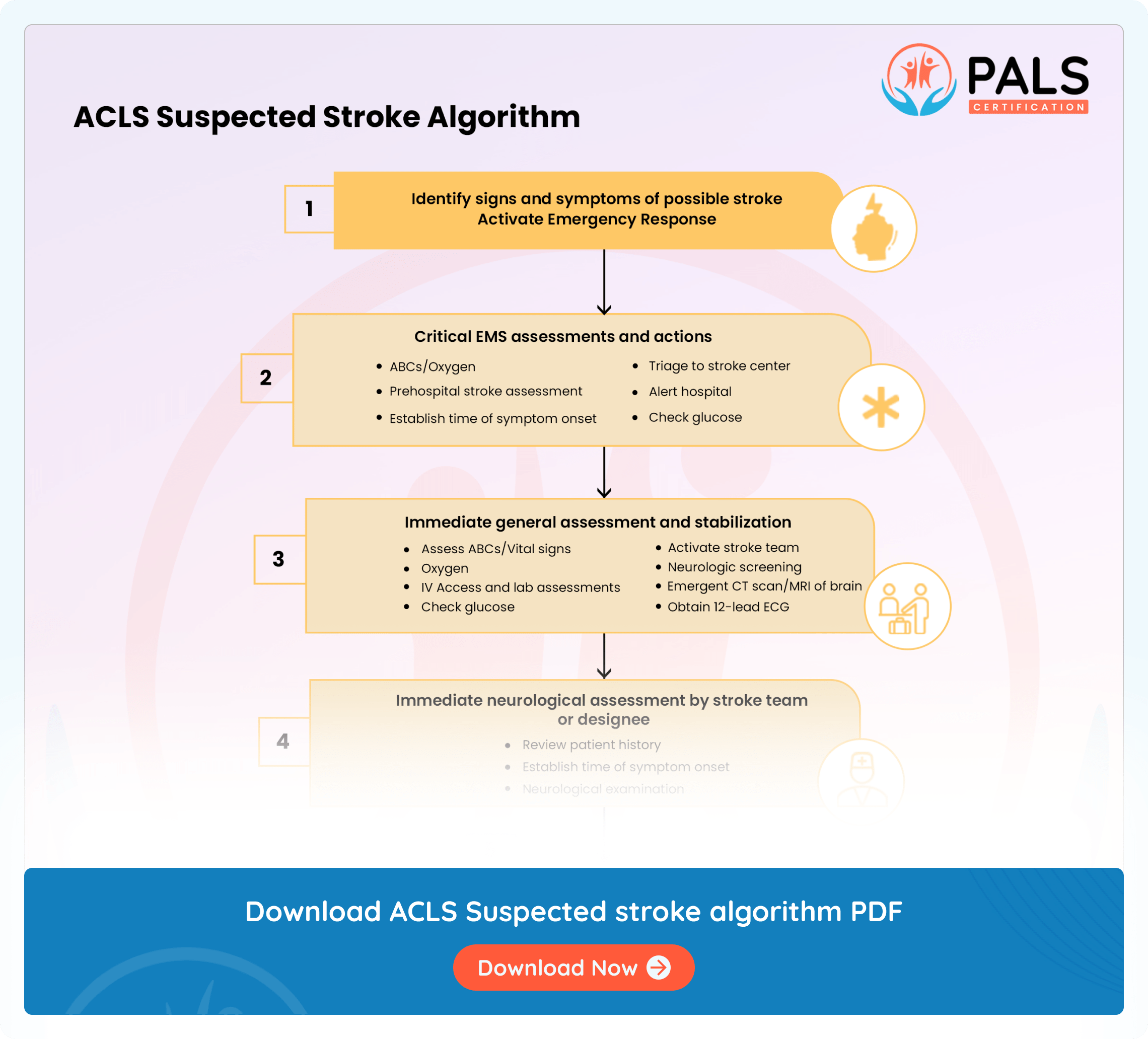
Step-by-step analysis of the flowchart
- Find out the signs and symptoms of a possible stroke and an active emergency response: Check the patient for signs of a stroke. Use F-A-S-T to find the warning signs such as facial drooping, arm weakness, speech difficulties, and time. The FAST acronym is an approach that allows healthcare providers and lay persons to easily identify if a patient is experiencing a stroke. Step 1. Ask the patient to smile. Does one side droop? Step 2. Ask the patient to close their eyes and raise both arms. Does one arm drift down? Step 3. Ask the patient to repeat a simple phrase. Does the patient’s speech seem slurred, garbled, or strange? Step 4. If you notice any of these symptoms, it is time to call the emergency responders. Please also notate the time the symptoms begin; this aids medical personnel to deliver the correct interventions. Call 911 immediately to activate the response system.
- Critical EMS assessments and actions: Assess for ABCs and support, if needed. Perform a prehospital stroke assessment and determine the stroke onset time. Visit the stroke center and alert the hospital well in advance to alert the stroke team. Consider a CT scan and check the glucose levels. If glucose is low, treat as indicated.
- Assess and stabilize: Perform a comprehensive assessment within 10 minutes. Inspect the vitals and offer oxygen to hypoxemic patients. Create IV access, run essential labs, and check the glucose levels; treat as indicated. At the same time, perform a neurologic screening with a CT scan or MRI of the brain.
- Neurologic assessment by stroke team: Engage the team to review the patient’s history and review the symptoms. Execute a detailed examination with the help of the NIH (National Institute of Health) Stroke Scale, or any other stroke scale your facility protocol utilizes. CT or MRI of the head should be completed within 20 minutes. Confirm the absence of hemorrhage on the CT scan prior to considering fibrinolytic therapy. Carefully examine for fibrinolytic exclusions, ensuring that you have a history of intracranial hemorrhage or head trauma excluded or have active internal bleeding excluded. Repeat the neurological exam to assess if the patient’s symptoms are improving, worsening, or staying the same. If there is hemorrhage on the scan, consult neurological experts and transfer the patient to a neurological ICU, if possible.
- Review benefits and risks with the patient and family: Discuss the risks and benefits of fibrinolytic therapy with the family and patient. This review must occur within 1 hour of arrival. Administer rtPA, also known as Recombinant Tissue Plasminogen Activator; it is a thrombolytic medication that dissolves clots that are obstructing blood flow to restore blood flow to the affected part of the brain.
- Post-rtPA stroke pathway: Initiate the post-rtPA stroke pathway within 3 hours of patient arrival. Admit patients to intensive care units and monitor their blood pressure for post-treatment care
The Advanced Cardiovascular Life Support (ACLS) suspected stroke algorithm is a framework for managing patients suspected of having a stroke. Here are the key components:
- Identification and Activation: The initial step recognizes stroke symptoms and triggers an emergency response. It utilizes the FAST method of Face, Arms, Speech, and Time to determine symptoms and intervene quickly. (3).
- Supportive Care: Implement comprehensive supportive care, maintain an open airway, ensure adequate breathing, and optimize systemic circulation.
- Timely Transportation: Seamless and timely transportation are fundamental. This increases the need for prehospital notification for swift intervention (1).
- Emergency Department Assessment: When a patient is first admitted, perform a rapid neurological evaluation, keeping in mind basic tests like blood glucose and a brain CT scan to differentiate between ischemic and hemorrhagic strokes (5).
- Stroke Team Evaluation and Typing: The stroke team performs a systematic investigation, identifies the stroke type, and, thus, works out a relevant treatment program (4).
- Ischemic Stroke Intervention: During ischemic strokes, timely treatment is critical within therapeutic windows. This helps prevent neuronal oxygen deficiency. Sometimes, in the clinical team, endovascular interventions are suggested (2).
- Hemorrhagic Stroke Management: During hemorrhagic strokes, interventions aim at controlling hypertension, reversing anticoagulation when applicable, and resorting to surgical treatment, if considered appropriate.
- Post-Acute Care Emphasis: Next, the focus changes to secondary prevention, rehabilitation, and management of complications. This holistic approach guarantees delivery of services both in the acute and other phases (6).
Available Courses
PALS Certification and Recertification Online
ACLS Certification and Recertification Online
- 4.0 - 8.0 CE Credit Hours
- For Healthcare Professionals
- Includes Videos, Megacode Scenarios, Practice Tests & More
$119.00 $169.00
Get CertificateBLS Certification and Recertification Online
- 6.0 CE Credit Hours
- For Medical Fields
- Includes CPR & First Aid Bag-Mask Techniques
$36.95 $39.90
Get CertificateSources
- Advanced vs. Basic Life Support in the Treatment https://linkinghub.elsevier.com/retrieve/pii/S0300957218301928
- van Walraven, C.; Stiell, I. G.; Wells, G. A.; Hébert, P. C.; Vandemheen, K. (November 1998). Do advanced cardiac life support drugs increase resuscitation rates from in-hospital cardiac arrest? The OTAC Study Group". Annals of Emergency Medicine. 32 (5): 544–553. doi:10.1016/s0196-0644(98)70031-9. ISSN 0196-0644. PMID 9795316. https://doi.org/10.1016%2Fs0196-0644%2898%2970031-9
- Jung, Julianna; Rice, Julie; Bord, Sharon (December 2018). "Rethinking the role of epinephrine in cardiac arrest: the PARAMEDIC2 trial". Annals of Translational Medicine. 6 (Suppl 2): S129. doi:10.21037/atm.2018.12.31. PMC 6330609. PMID 30740450. https://doi.org/10.21037%2Fatm.2018.12.31
- ACLS Traditional Acute Stroke https://anesthesia.ucsf.edu/sites/anesthesia.ucsf.edu/files/wysiwyg/AcuteStroke.pdf
- Perkins, Gavin D.; Gräsner, Jan-Thorsen; Semeraro, Federico; Olasveengen, Theresa; Soar, Jasmeet; Lott, Carsten; Voorde, Patrick Van de; Madar, John; Zideman, David; Mentzelopoulos, Spyridon; Bossaert, Leo (2021-04-01). "European Resuscitation Council Guidelines 2021: Executive summary". https://www.resuscitationjournal.com/article/S0300-9572(21)00055-1/abstract
- Resuscitation. 161: 1–60. doi:10.1016/j.resuscitation.2021.02.003. ISSN 0300-9572. PMID 33773824. S2CID 232407605. https://doi.org/10.1016%2Fj.resuscitation.2021.02.003
All PALS Algorithms
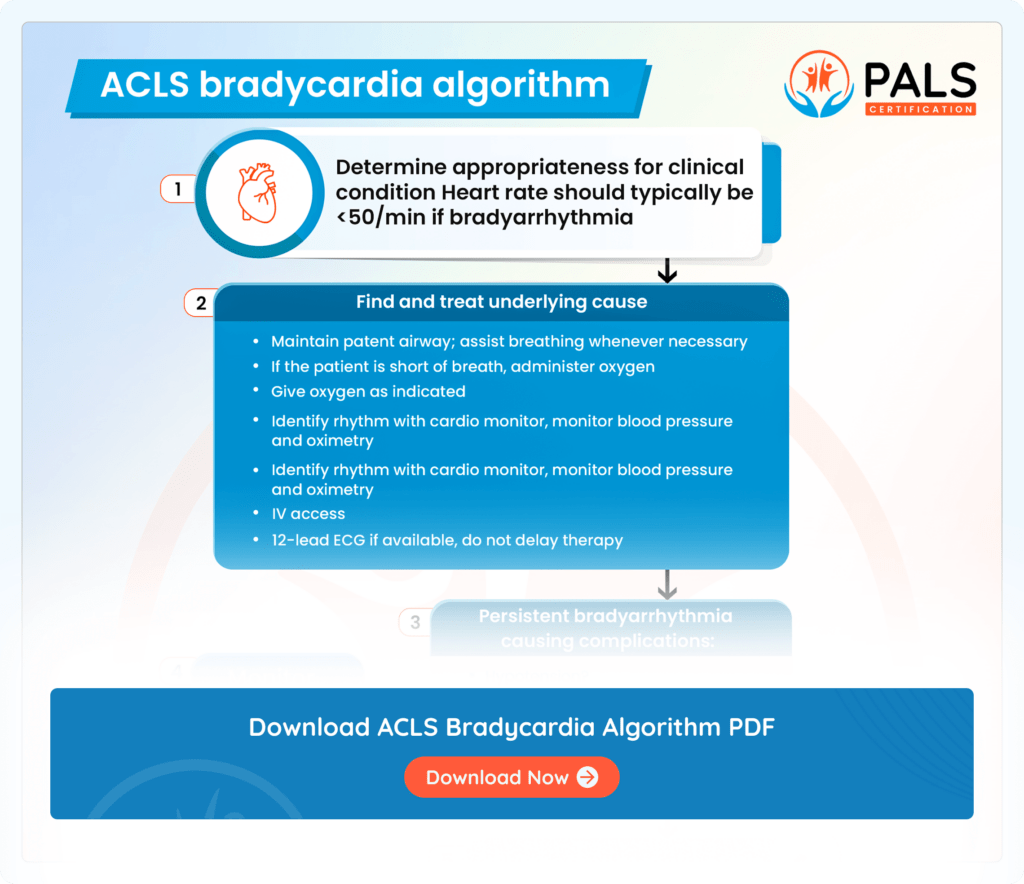
ACLS Bradycardia Algorithm
An ACLS Bradycardia algorithm helps you learn the guiding interventions for emergency slow heart rates
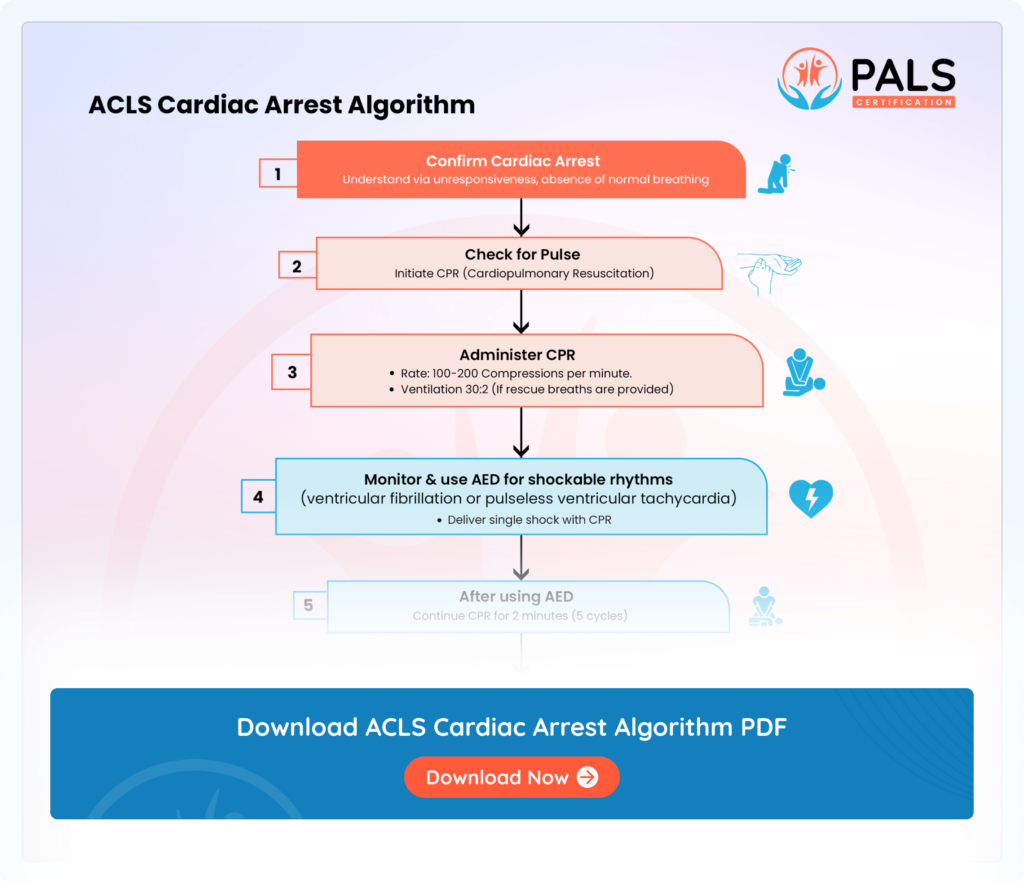
ACLS Cardiac Arrest Algorithm
The ACLS cardiac arrest algorithm directs resuscitation efforts, outlining steps like patient assessment, CPR initiation, defibrillation if needed, medication administration, reversible cause evaluation, and advanced interventions.
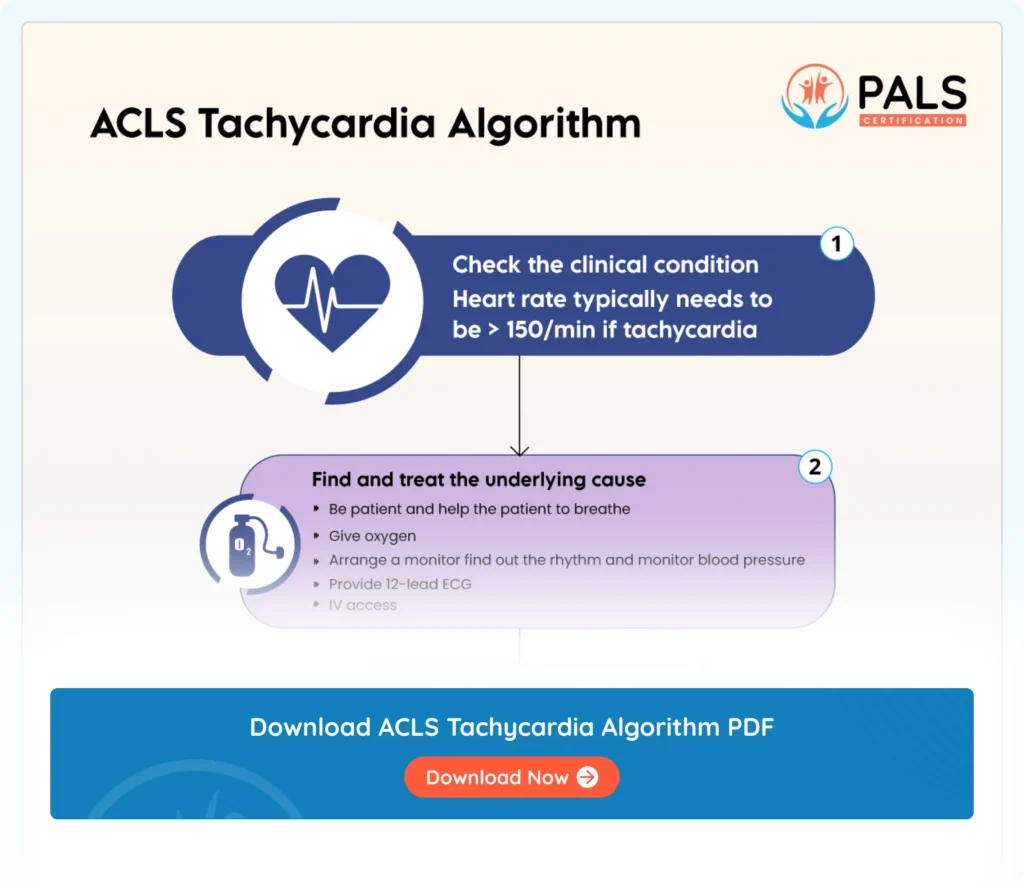
ACLS Tachycardia algorithms
ACLS tachycardia algorithm helps manage elevated heart rates through systematic interventions for optimal patient outcomes