Identifying and Treating Second-Degree AV Block Type I (Wenckebach or Mobitz Type I)
Did you know that, according to the Centers for Disease Control and Prevention (CDC), arrhythmias affect over 2.7 million Americans each year? It is essential to understand Wenckebach, as it involves the electrical system of the heart. This impacts its ability to beat efficiency, causing second degree atrioventricular block. The blog explores the intricacies of the rhythm and deciphers its symptoms, causes, and treatments that bring the rhythm back. Keep reading to explore second-degree AV block type I, uncover the symptoms, and identify the root causes.
What is ventricular fibrillation?
Ventricular fibrillation (VF) is a life-threatening cardiac arrhythmia characterized by rapid, chaotic contractions of the heart’s ventricles. The heart’s electrical signals get disorganized and contract effectively. This activity hinders the ability of the heart to pump blood and leads to a rapid decline in blood circulation.
Any delay in providing treatment, such as defibrillation, to reform the normal rhythm of the heart can be fatal, even within a few minutes. The factors that predispose to ventricular fibrillation are prior coronary artery disease, myocardial infarction, heart failure, and important electrolyte disorders. The recognition of the incidence and the prompt treatment of ventricular fibrillation are key to the management of the condition and the patient’s chances of surviving. Automated external defibrillators (AEDs) are critical devices used in the timely delivery of lifesaving shocks to bring back a normal heart rhythm during medical emergencies.
How do you identify the cardiac rhythm of a patient with ventricular fibrillation?
Identifying ventricular fibrillation (VF) in a patient involves assessing the cardiac rhythm through several means. Explore the steps to help identify VF:
- Monitor: Use a portable cardiac monitor to continuously document the patient’s heart rate and rhythm. Arrange the electronic instrument so that the monitor displays the irregular, chaotic waveforms.
- Check Pulse: Check for a pulse presence. In ventricular fibrillation, a quivering heart is the case. Pulse is often weak or absent. If there are no beats, start CPR instantly.
- Clinical Signs: Monitor the patient for any signs of rapid collapse, loss of consciousness, or breathing irregularities.
- Electrocardiogram (ECG or EKG): Perform an ECG for a total of 12 leads in order to observe the heart’s electrical activity in detail. Seek the pattern illustrated by irregular and chaotic waveforms in ventricular fibrillation.
- Automated External Defibrillator (AED): When possible, utilize an AED to assess the heart rhythm. AEDs can detect ventricular fibrillation and can autonomously deliver a shock to recover a normal rhythm.
- Medical History: Think of the patient’s medical background, as underlined heart conditions or a history of cardiac events may represent important risk factors for developing the condition of ventricular fibrillation.
- Clinical Assessment: Evaluate the overall clinical state of the patient by performing a physical exam, including the patient’s status of skin color, responsiveness, and whether the patient is using mind control or not.
If VF is suspected, start CPR and use an AED as quickly as possible. It is therefore essential to prioritize early defibrillation to improve the chances of survival in patients with ventricular fibrillation.
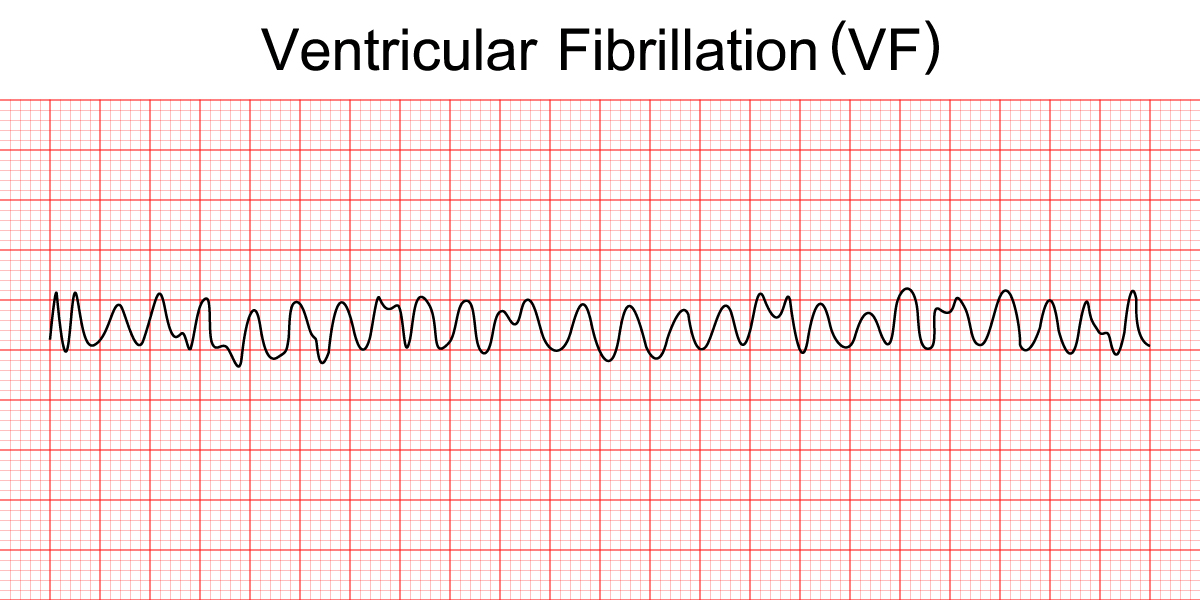
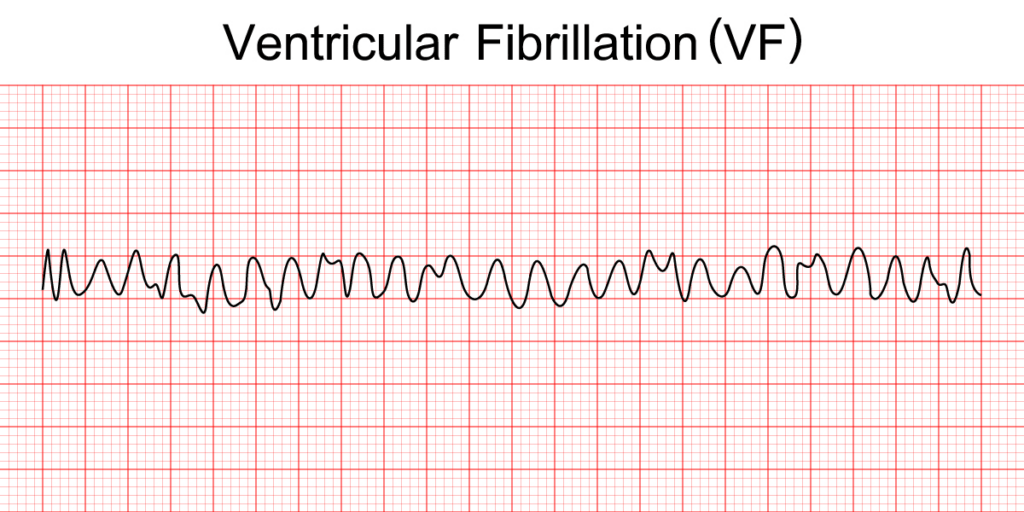
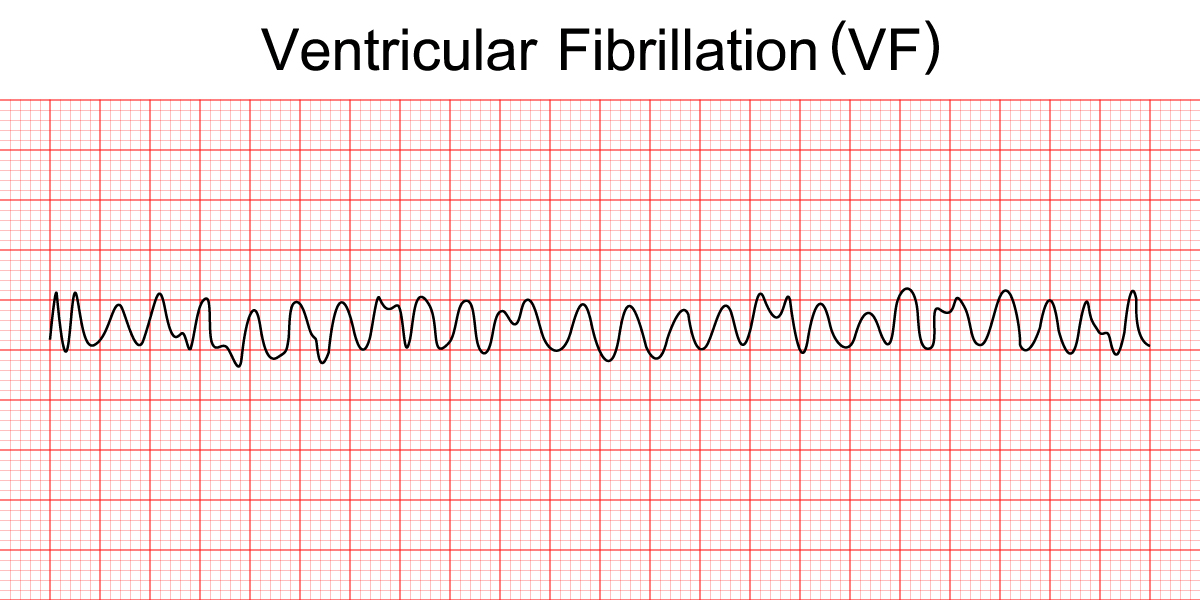
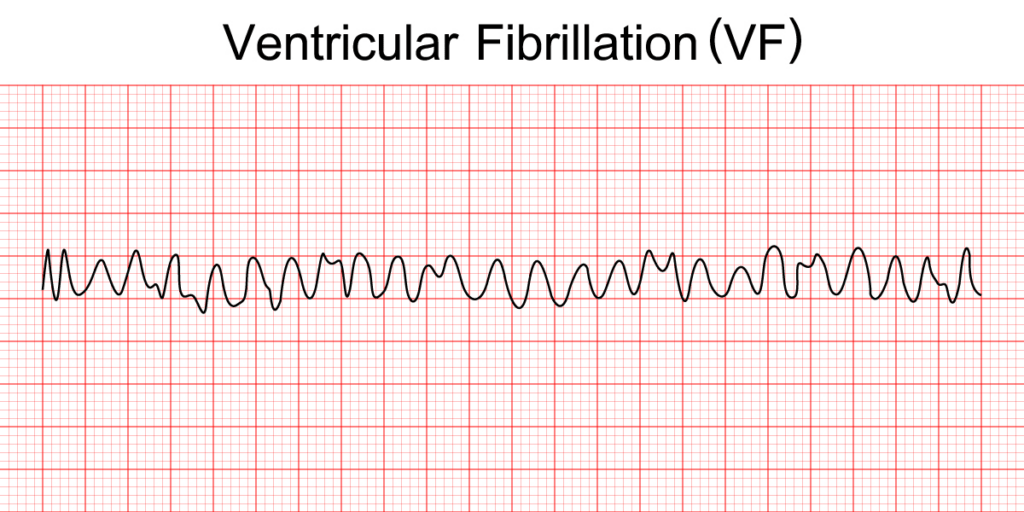
ECG pattern and key features
The electrocardiogram (ECG or EKG) is a crucial tool that assesses the electrical activity of the heart. In ventricular fibrillation (VF), the ECG pattern is characterized by irregular waveforms. Key features of the ECG pattern:
- Absence of Regular Rhythm: VF refers to the irregular heartbeat, which results in a lack of rhythm. Thus, instead of normal right-sided P waves or T waves, which are usually observed in an ECG, this demonstrates a disorganized and chaotic picture.
- Irregular Waveforms: The ECG tracings of VF units exhibit fine, irregular, or coarse oscillations with fibrillatory waves.
- No Discernible QRS Complex: In VF, there is no recognizable QRS complex, which is a precipitating condition of organized ventricular contractions. Thus, the ventricles contract; however, the contractions are usually not as strong as they ought to be.
- No Clear P Waves: There is no possibility of separating P waves, representing atrial depolarization, in the VF due to the chaotic nature of the activity.
- Baseline Wander: The baseline involves irregular waving due to the disparate signals produced by the quivering ventricles.
- Flat Line: In certain areas of the ECG, it showcases an undeviating or almost undeviating state due to the lack of any integral electrical activity.
- Confirmation with 12-Lead ECG: A 12-lead ECG will enhance the overall picture, revealing the absence of a regular rhythm.
Physical symptoms
Ventricular fibrillation (VF) disrupts the normal pumping function. Although VF does not present with physical symptoms, its consequences can manifest broader signs of cardiovascular collapse. The symptoms involve the following:
- Loss of consciousness
- No pulse or weak pulse
- Rapid and shallow breathing
- Pale skin
- Dilated pupils
- Cold skin
What are the causes of ventricular fibrillation?
Ventricular fibrillation is a result of underlying heart conditions that disrupt the signals regulating the heart’s rhythm. The common causes include the following:
- Coronary Artery Disease (CAD): Arteries can get narrowed, leading to a reduction of blood flow to the heart, resulting in VF.
- Myocardial Infarction (Heart Attack): In a heart attack, scar tissue formed from the impacted heart can prevent the heart muscle from contracting appropriately, resulting in VF.
- Heart Failure: The weakened heart muscles affect the contracting of the heart, which limits the heart’s function of pumping blood, thereby risking the chance of VF.
- Cardiomyopathy: Weakening of the heart muscle due to the conditions involved makes a person more susceptible to VF.
- Congenital Heart Defects: Impairments that a neonate may be born with may potentially cause an interruption of the heart’s rhythm and thereby provoke VF.
- Electrical Abnormalities: Long-QT syndrome or Brugada syndrome could result in ventricular fibrillation.
- External Factors: The VF may ensue from severe electrolyte imbalances, drug toxicity, or electric shock.
- Immediate Defibrillation: VF typically requires prompt emergency medical intervention, which may involve the use of an electrical shock to restore normal heart activity.
Prior conditions
VF can quickly develop from unstable VT, and the methods are similar for the critical conditions. It is due to a lack of blood or oxygen to the heart muscle.
Reversible causes
Although some factors inducing VF are irreversible, the causes are reversible. After the patient reaches a non-shockable rhythm, you need to treat hypoxia, pulmonary thrombosis, and several other causes.
Treatment
The first step of treatment focuses on rapid termination, providing an immediate restoration of blood flow to crucial organs. However, before taking any steps, defibrillate immediately and administer oxygen without manual ventilation. If a defibrillator is not present, start CPR as soon as possible. As soon as the defibrillator arrives, access the ECG with the help of adhesive chest patches.
- CPR and IV infusion: Prioritize immediate defibrillation and administer high-quality CPR. Perform 2-inch chest compressions at 100–120 per minute and compress 1/3 of the chest’s anteroposterior dimension. As it is the primary goal, CPR temporarily sustains the blood flow. Establish IV access and ensure swift intervention.
- Defibrillation: Both undulous VT and VF are fibrillation rhythms that require a quick DC electric shock. Apply 360 joules for monophasic devices and 120–200 joules for biphasic devices. Follow your defibrillator’s recommendations. (And if the first shock fails, perform CPR and the indicated drugs.) Re-recommend defibrillation and CPR until we have been unable to produce a shockable rhythm.
- Post-treatment prevention: This permits preventive interventions. ICD insertion (a ventricular fibrillation detector and defibrillator) as recommended by electrophysiologists is beneficial for high-risk patients. ICDs are not useful for VF that is caused by reversible factors. Catheter ablation, although infrequent, helps abstain from VF via the elimination of heart regions that cause impulse deviations. The procedure also serves as an option when the medicines prove ineffective or impractical. Both therapies strengthen patient safety through the identification and management of underlying risks related to VF and also design personalized programs for those with a recurrent risk of life-threatening fatal arrhythmias.
Conclusion
Ventricular fibrillation is a critical condition that needs treatment, as it can end up in asystole and death. To boost the survivability of the patient, take quick action and increase the chances of their survival. Along with CPR and drugs, the above-mentioned steps synchronize and restore the patient to a stable condition and proper rhythm.
PALS CERTIFICATION
Author
PALS Certification is a trusted provider of online life support training, offering PALS, BLS, and ACLS certification and renewal courses. Our flexible training programs follow industry guidelines, offer self-paced learning and instant certification, ensuring providers stay compliant, advance their credentials, and deliver high-quality patient care.