- 4.0 CE Credit Hours
- For Pediatric Responders
- Includes Videos, Megacode Scenarios, Practice Tests & More
- FREE BLS Included
The ACLS tachycardia algorithm functions as a structured guide and provides healthcare providers with a systematic approach to handling patients experiencing a heart rate exceeding 150 beats per minute. This algorithm is ideal for adults and ensures a strategic response to tachycardia, emphasizing the need for precise interventions to optimize medical outcomes.
It enables healthcare professionals to navigate through the algorithm when confronted with an adult patient exhibiting tachycardia. These procedural steps ensure adequate perfusion and initiate synchronized cardioversion while administering antiarrhythmic medications. This facilitates timely interventions and enhances patient outcomes. Here is the step-by-step flowchart for the ACLS tachycardia algorithm.

Online PALS certification and recertification
- Compliant with ECC and OSHA guidelines
- Nationally accepted course
- Available anytime, anywhere
- Earn CE credit hours
$119
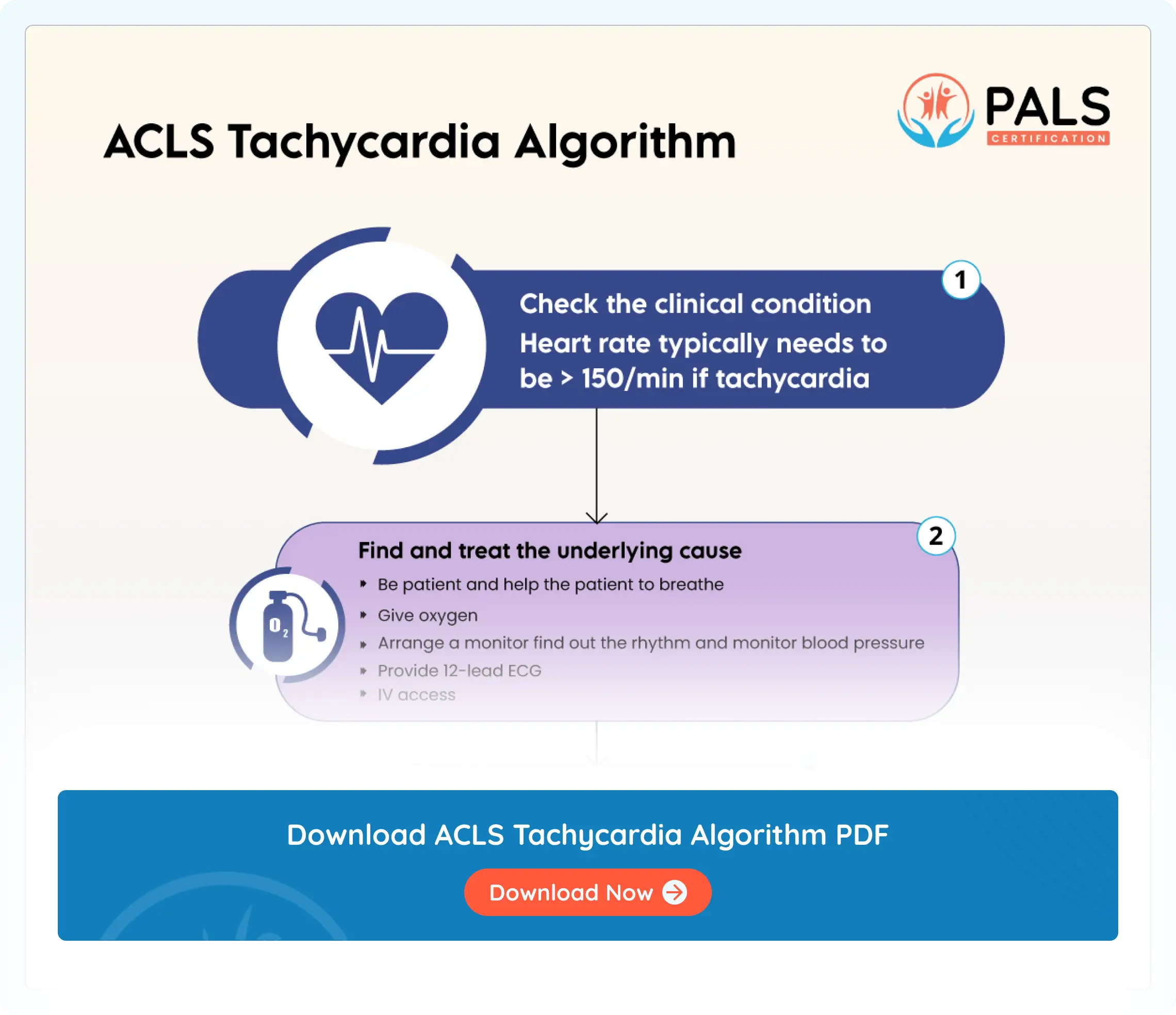
Explanation of the flowchart
- Evaluate suitability for clinical presentation and intervention
- Ascertain if the heart rate exceeds 150 beats per minute, indicating the presence of tachycardia.
- If yes, then proceed to the next step.
- Identify and address the root cause
- Uncover and manage potential factors contributing to tachycardia.
- Ensure an obstructed airway and support the patient’s breathing.
- If the patient is hypoxemic, then provide oxygen.
- Cardiac monitoring
- Employ a cardiac monitor to discern the rhythm and monitor blood pressure and oxygen saturation.
- Perform a 12-lead ECG, if accessible.
- Establish intravenous (IV) access in anticipation of potential interventions. Remember, if IV access is unobtainable, Intraosseous (IO) vascular is the next consideration.
- Check for complications stemming from persistent tachyarrhythmia
Check whether persistent tachyarrhythmia is a result of complications such as hypotension, indications of shock, or heart failure. - If hypotensive, then:
- If yes, then utilize interventions for wide QRS complexes.
- For a monomorphic rhythm, consider adenosine.
- Address the underlying cause if refractory, escalating energy levels during cardioversion, and adding anti-arrhythmic drugs while seeking expert consultation.
- Is QRS wide? Greater than or equal to 12 seconds?
- Adenosine is a consideration only if the rhythm is regular.
- If refractory, ponder addressing the underlying cause, escalating energy levels during cardioversion, adding anti-arrhythmic drugs, and seeking expert consultation.
- If negative, consider vagal maneuvers (if the rhythm is regular), adenosine, β-blockers, or calcium channel blockers, and seek advice from medical experts.
Key components of the ACLS tachycardia algorithm include:
- Early detection and prompt action: Healthcare providers play a crucial role in recognizing signs of tachycardia. This swiftly activates the ACLS tachycardia algorithm and initiates the emergency response system when needed.
- Evaluation and basic life support: An assessment of the patient’s stability guides appropriate interventions for wide-complex and narrow tachycardia. Basic life support includes tailored actions and employs the right anti-arrhythmic drugs based on individual needs.
- Advanced cardiovascular life support (ACLS): If patient stability is compromised, then you must offer synchronized cardioversion along with antiarrhythmic drugs. Additionally, you must seek expert consultation whenever necessary.
- Identification and resolution of reversible causes: Addressing and recognizing factors such as hypoxia and electrolyte imbalances is crucial for effective management and improvement of patient outcomes.
- Post-tachycardia care: It is crucial to initially administer before interventional stabilization. Tachycardia care transitions post-treatment, following stabilization and intervention. This process involves continuous monitoring, finding underlying causes, and adopting best practices for patient outcomes.
- Recovery measures: Hospitals may implement strategies such as placing patients in a recovery position. This helps maintain closed airways and prevents inhalation for unconscious patients.
- Refractory situations: Refractory scenarios take place when tachycardia does not respond to initial treatment. Aggressive interventions are necessary for timely condition management.
- Wide QRS: A wide QRS can be associated with fast heart rhythm. An electrocardiogram (ECG) can help demonstrate the duration of the QRS complex. A wide QRS complex is greater than or equal to 12 seconds. This indicates an abnormal origin of the electrical impulse.
- Synchronized cardioversions: Synchronized cardioversion aims at restoring a normal heart rhythm in individuals experiencing abnormal heart rhythms, especially tachycardias. This procedure delivers a timed electrical shock to the heart and allows the natural pacemaker to create a regular heartbeat.
Available Courses
PALS Certification and Recertification
ACLS Certification and Recertification
- 6.0 CE Credit Hours
- For Healthcare Professionals
- Includes Videos, Megacode Scenarios, Practice Tests & More
- FREE BLS Included
$119.00 $169.00
Get CertificateBLS Certification and Recertification
- 6.0 CE Credit Hours
- For Medical Fields
- Includes CPR & First Aid Bag-Mask Techniques
$36.95 $39.90
Get CertificateSources
- Advanced Cardiovascular Life Support Algorithms. Retrieved from https://www.ahajournals.org/doi/10.1161/circ.102.suppl_1.I-136
- Proper post-resuscitation care (PRC) has been shown to reduce mortality and morbidity. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4237286/#bib1
- Successful termination of the tachycardia by vagal maneuvers suggests AVNRT or CMT by an accessory pathway, whereas syncope suggests rapid SVT, atrial fibrillation with conduction over an accessory pathway, or concomitant structural cardiac abnormalities. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884443/
- Synchronized cardioversion is a procedure similar to electrical defibrillation in that a transthoracic electrical current is applied to the anterior chest to terminate a life-threatening or unstable tachycardia arrhythmia https://www.ncbi.nlm.nih.gov/books/NBK482173/
- The most frequent reversible causes of CA with PEA as initial rhythm are commonly referred to by the mnemonic “4 Hs and 4Ts”: hypoxia, hypovolemia, hypo/hyperkalemia, hypo/hyperthermia, cardiac tamponade, tension pneumothorax, thrombosis, and toxins. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9485947/#B3
- A 2015 ILCOR Consensus on Science on this topic concluded that first aid providers should position unresponsive persons who are breathing adequately into a recovery position. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9065878/
- A normal QRS should be less than 0.12 seconds (120 milliseconds), therefore a wide QRS will be greater than or equal to 0.12 seconds. https://www.uptodate.com/contents/advanced-cardiac-life-support-acls-in-adults
- A normal QRS should be less than 0.12 seconds (120 milliseconds), therefore a wide QRS will be greater than or equal to 0.12 seconds. https://www.ncbi.nlm.nih.gov/books/NBK559054/#:~:text=A%20normal%20QRS%20should%20be,or%20equal%20to%200.12%20seconds
- Cardio Procedure threating https://pubmed.ncbi.nlm.nih.gov/29489237/#:~:text=Synchronized%20cardioversion%20is%20a%20procedure,threatening%20or%20unstable%20tachycardic%20arrhythmia
All ACLS Algorithms
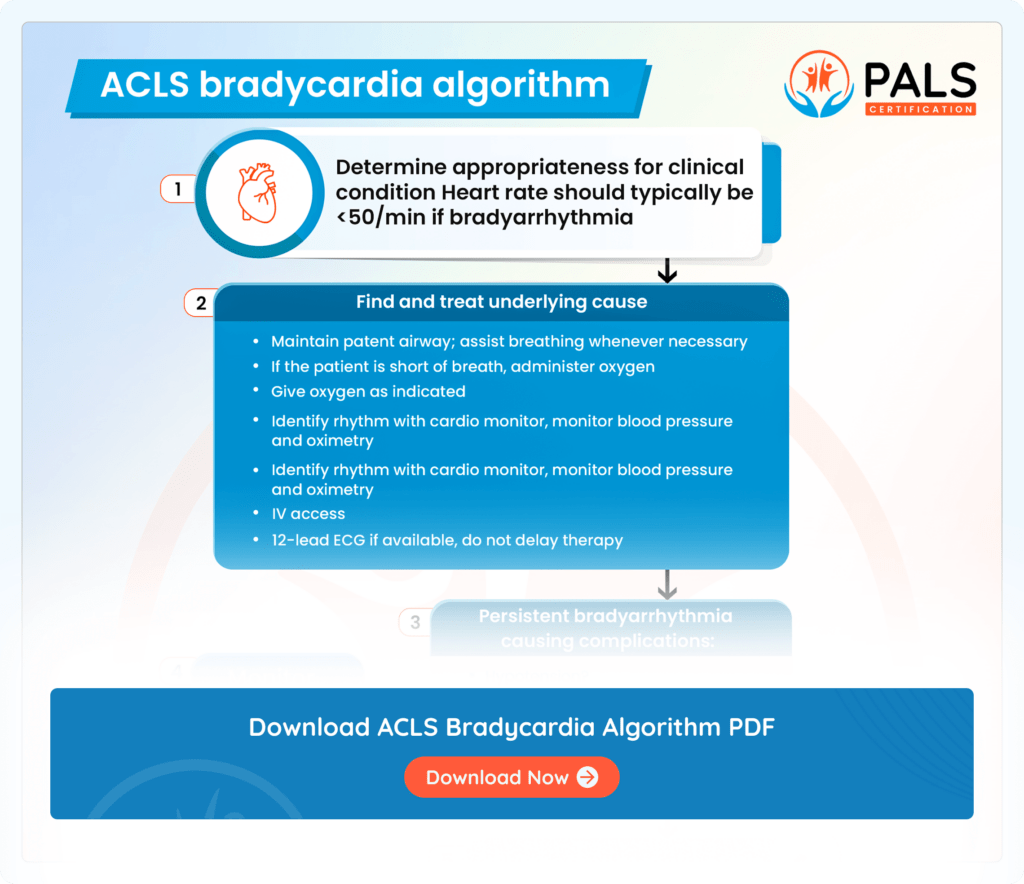
ACLS Bradycardia Algorithm
An ACLS Bradycardia algorithm helps you learn the guiding interventions for emergency slow heart rates
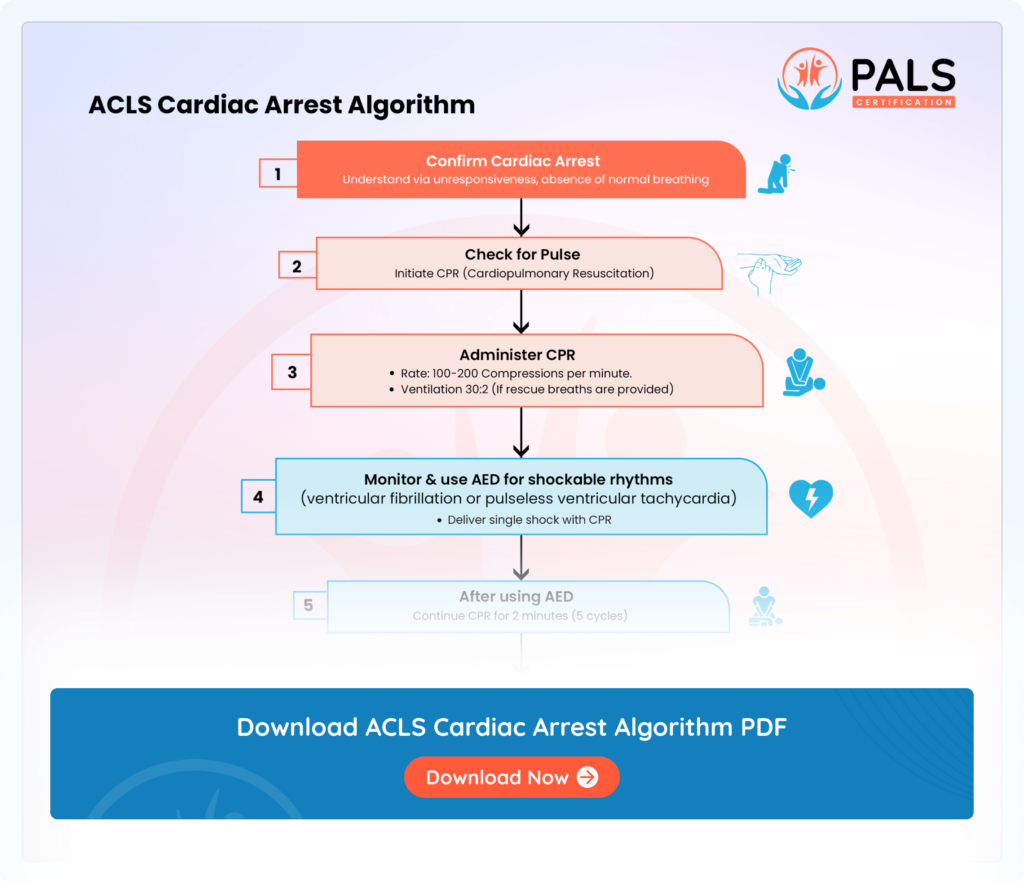
ACLS Cardiac Arrest Algorithm
The ACLS cardiac arrest algorithm directs resuscitation efforts, outlining steps like patient assessment, CPR initiation, defibrillation if needed, medication administration, reversible cause evaluation, and advanced interventions.
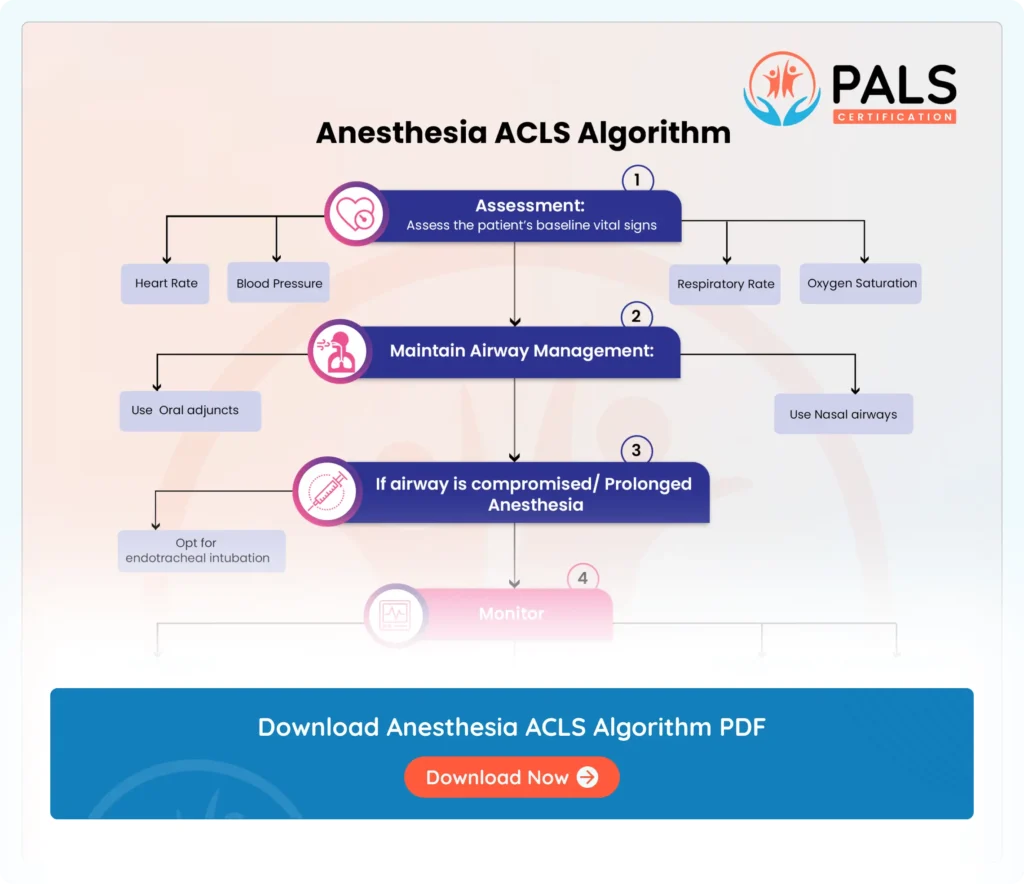
Anesthesia ACLS Algorithm
Know how to assess vital signs, secure airway and initiate CPR when needed. Administer ACLS drugs, address reversible causes and adapt management to patient’s condition for anesthesia emergencies.


